by Assistant Professor Chalermchai Mitrpant, MD, PhD, Department of Biochemistry
Obesity-related glomerulomegaly (ORG) is a condition characterized by the following histopathological features:
- Enlargement of the glomerulus.
- Widening of the mesangial matrix, an increase in mesangial cell number, and dilation of capillaries.
- Hypertrophy of podocytes, the glomerular filtration cells.
ORG, a silent pathological condition, is observed in approximately 0.2% of individuals with obesity. Over the past two decades, the global increase in obesity due to dietary and lifestyle changes has led to a significant rise in ORG prevalence. This condition typically remains asymptomatic for years until kidney function declines, potentially progressing to chronic kidney disease (CKD) or end-stage renal failure. Among CKD patients, 15–30% also present with ORG.
The zebrafish (Danio rerio), a vertebrate with genetic and physiological similarities to humans, has been widely employed in biomedical research. In this study, we developed a diet-induced obesity (DIO) zebrafish model to investigate ORG. Histopathological analysis of zebrafish kidney tissues revealed glomerular enlargement consistent with ORG in humans. Additionally, changes in proximal tubule cells and focal segmental glomerulosclerosis (FSGS) were observed.
Gene expression profiling of kidney tissues from experimental zebrafish showed upregulation of genes associated with inflammation, fibrosis, and lipid metabolism. These findings suggest that this model is a valuable tool for elucidating the molecular mechanisms underlying ORG.
Future research can leverage advanced technologies, such as DESI-Imaging Mass Spectrometry (DESI-IMS), to analyze the spatial distribution of small biomolecules, including lipids, within affected tissues. Moreover, epigenomic approaches combining diverse omics datasets—such as ATAC-sequencing for chromatin accessibility analysis, histone modification profiling, and RNA sequencing—can provide insights into the regulatory networks governing gene expression in diseased versus healthy kidney tissues.
Comprehending the pathophysiological mechanisms of ORG will pave the way for preventive strategies and innovative therapeutic approaches in kidney disease management.
by Lecturer Nattapong Polharn, CPO, Sirindhorn School of Prosthetics and Orthotics
Patients with hemiplegia often face mobility challenges, such as foot drop and equinovarus (inward ankle twisting), resulting in instability while walking, increased energy expenditure, and a higher risk of falls—particularly on uneven surfaces. Conventional ankle-foot orthoses (AFOs) partially address these issues but lack the flexibility for natural movement.
This research introduces a newly developed, patented ankle joint capable of bi-planar motion, allowing movements in both the sagittal plane (dorsiflexion/plantarflexion) and the frontal plane (inversion/eversion). The device is further enhanced with an internal shock-absorbing system to improve stability on uneven terrains. This innovative design aims to restore stable and natural-like walking for hemiplegic patients.
Importance of Bi-Planar Motion and Shock Absorption
Lateral ankle movement plays a critical role in maintaining balance on uneven surfaces. Restricted motion in this plane increases torque on the knee and hip joints, leading to higher energy demands, greater instability, and an elevated fall risk. Additionally, shock absorption during the heel-strike phase of walking is crucial for reducing joint stress and ensuring smooth gait transitions.
Traditional AFOs, such as Tamarack joints and AFOs with oil dampers, have limitations in supporting bi-planar movement and providing adequate shock absorption in all scenarios. These constraints make walking, especially on uneven surfaces, challenging for users of these devices.
Features and Design of the Patented Joint
The patented joint incorporates dual-axis rotation, enabling motion in both sagittal and frontal planes. It also includes an adjustable spring-based shock absorption system tailored to patient needs. Constructed from high-quality stainless steel, the joint offers durability for long-term use.
Performance testing compared the patented joint to conventional AFOs by evaluating parameters such as walking speed, center of gravity (COG) movement, and ground reaction force (GRF) patterns on both even and uneven surfaces.
Impressive Results
The patented joint demonstrated superior performance, significantly enhancing stability and walking speed. Key findings include:
- COG Movement: The new joint ensured smooth and balanced COG shifts between left and right sides.
- Walking Speed: Patients achieved the highest walking speeds using the new joint, with average speeds on uneven surfaces exceeding those with other devices.
- Shock Absorption: The internal spring system effectively reduced impact forces during heel strikes, resulting in smoother gait transitions and minimized stress on other joints.
This groundbreaking development offers a promising solution for hemiplegic patients, enabling more stable and natural mobility across diverse terrains.
IMPORTANCE OF CADAVERS IN MEDICAL EDUCATION
Cadavers are invaluable in medical education, allowing students to study, learn, and practice medical procedures before performing them on actual patients. These procedures require mastery and expertise, and cadavers provide a crucial hands-on experience for developing these skills.
INTEGRATION OF MEDICAL SIMULATORS
To enhance the training process, medical simulators were introduced, developed in collaboration with the Siriraj Medical Education Technology Center. These artificial skin models closely resemble human skin, allowing students to practice injections in a realistic environment before moving on to cadavers.
TRADITIONAL PRACTICE METHODS
In the past, medical students practiced procedures using fruit skins, such as cutting a banana peel or peeling tomato skin without damaging the inner flesh. This practice, known as the “Fruit Lab,” became a part of the residency training curriculum at the Department of Dermatology, Faculty of Medicine Siriraj Hospital, Mahidol University.
CURRENT USE OF CADAVERS
Cadavers are used monthly to teach dermatological procedures, particularly aesthetic ones like botulinum toxin and filler injections. However, since these procedures primarily focus on the face, it results in the overuse of cadavers. The belief is that cadavers should be preserved for procedures with greater medical significance.
REDUCING CADAVER RELIANCE WITH TECHNOLOGY
To minimize cadaver use, we have explored technological alternatives. In 2019, a collaboration with SurgiMind Co., Ltd. from South Korea led to the development of the “Anatomy 2D-3D” program. Initially starting as a 2D anatomy program, it has evolved into a 3D platform with a 360-degree view, simulating cadaver dissections by visualizing and dissecting facial layers.
INTRODUCTION OF MIXED REALITY (MR)
Recent advancements include the integration of Mixed Reality (MR) technology, combining Virtual Reality (VR) and Augmented Reality (AR). Using hologram glasses, learners can interact with 3D virtual objects in real space, providing a more realistic and immersive practice experience.
FUTURE DEVELOPMENT PLANS
Plans are underway to expand this technology for other procedures such as injections and thread lifts. As an online program, it holds international potential, offering Mahidol University students free access to these learning resources. Additionally, the program is being developed into an interactive game where students can earn points while learning, making the educational process more engaging.
IMPACT AND CONTRIBUTION
This innovative project not only advances medical education but also offers valuable research opportunities. It supports the mission of the Faculty of Medicine Siriraj Hospital, Mahidol University, in fostering education, research, innovation, and medical services. By contributing to society and strengthening the university’s reputation as the “Medical Institution of the Land,” the project enhances
global healthcare through knowledge generation and improved medical practices.
By Assoc. Prof. Natthawut Sermsathanasawadi, M.D., Ph.D. Varicose veins are a common medical condition where patients may experience symptoms such as leg pain during walking or standing for long periods, leg swelling, cramps, itching, and visible large varicose veins. The skin on the legs may become darker, and in severe cases, ulcers may form around […]
Inguinal hernia is a common disease in general medical practice. It can occur in both males and females and requires surgical treatment. Annually, a large number of patients undergo hernia repair surgery at Siriraj Hospital. However, giant inguinal hernia is much rarer due to its definition: a hernia extending below the midpoint of the inner thigh when the patient is standing. This condition results from patients leaving the hernia untreated for a long time. Nowadays, with improved and accessible healthcare services, patients receive treatment earlier, making this condition less common.
Giant inguinal hernia is found exclusively in males and is significantly more complex and difficult to treat compared to regular inguinal hernias. The complication rate is high, with literature reviews indicating a 40% complication rate in patients undergoing surgery for giant inguinal hernia. Historically, there have been reports of deaths due to the sudden and significant increase in intra-abdominal pressure when returning the herniated organs, which had been outside the abdominal cavity for a long time, back into the cavity, leading to respiratory failure.
Due to the rarity and complexity of giant inguinal hernia, most medical reports are case reports, lacking a classification system or standardized surgical recommendations. In 2014, Assoc. Prof. Atthaphorn Trankarnsanga, M.D., FRCST., and colleagues from the Minimally Invasive Surgery Unit, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, developed a classification system for giant inguinal hernia. This system divides the disease into three types based on the size of the hernia sac and proposes corresponding treatment methods. The system was published in an international medical journal and has been cited in over 60 medical journals and international conference lectures.
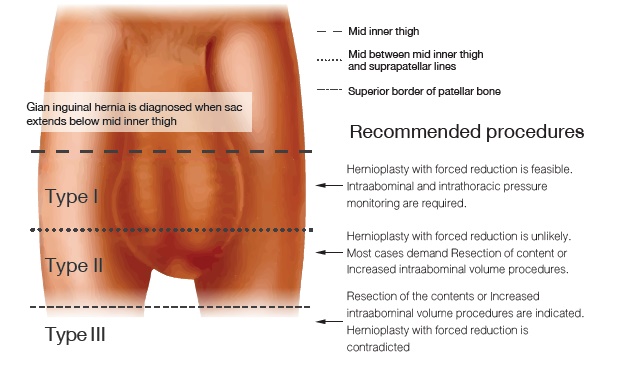
In 2024, the authors conducted a literature review and meta-analysis to verify the accuracy of this classification system. They found that for type I giant inguinal hernia, all 66 reported cases were successfully treated according to the recommended guidelines. For types II and III, among 33 cases, eight patients did not receive treatment according to the classification recommendations, resulting in severe complications in 36% of these cases, including abdominal compartment syndrome and pulmonary embolism. However, there were no reported deaths, demonstrating the accuracy of the classification system developed by Siriraj.
This achievement is a source of pride for Siriraj, reflecting its longstanding commitment to academic research that benefits patient care, both in Thailand and internationally. This aligns with Siriraj’s 2024 concept of “we are ready” and exemplifies the “ready to discover” initiative.